In my last post I talked about our hope that by sharing stories widely, we can help to engender learning and change in services.
But a simple search of providers on Patient Opinion shows that there's no automatic connection between the amount of feedback and the amount of (visible) change.
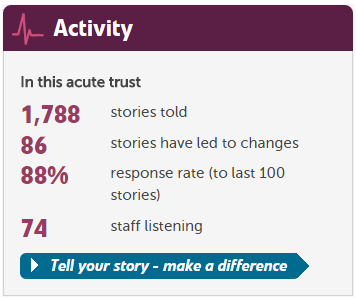
For example, at Surrey and Sussex Healthcare, there's plenty of feedback and a fair amount of change as a result:
Meanwhile, not far away at the Royal Surrey County Hospital, there's a third of the amount of feedback - with no visible changes at all.
Why is it hard to make changes as a result of patient feedback?
A recent paper by Laura Sheard, Claire Marsh and colleagues at Bradford Institute of Health Research, based on observing 17 ward-based staff teams, helps to explain why.
Over a period of six months, staff worked with feedback from patients about safety issues on their wards. Some teams were able to use the feedback to initiate changes, while other teams did not use it, or tried to make changes but failed.
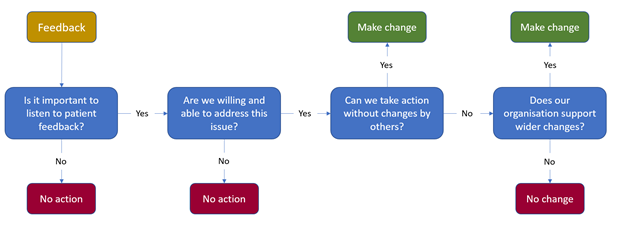
The authors developed a model (the "patient feedback response framework") to describe what was needed for change to occur. I've taken the liberty (with permission) of summarising the model into a simple flowchart.
(A larger image is available.)
Although the flowchart is simple, it makes clear what is needed for feedback to lead to change. Staff must feel that patient feedback is worth acting on. They must feel both willing and able to do so. If they have control over the changes needed, they may then go ahead.
But hospitals are complex places and many improvements will require others to make changes too. And if the organisation does not permit or encourage that kind of wider change, or if other teams in turn are unable or unwilling to make changes, then nothing will happen.
Given this context it is remarkable that we see as many changes as we do on Patient Opinion. And it also prompts us to ask: how could we develop Patient Opinion further in ways which would support the likelihood of change?
Finally, I would highlight a warning from Sheard and colleagues which resonated strongly with me:
"We believe that until ward staff are given robust organisational support to implement changes then the value of Trusts collecting patient feedback is questionable."
Why do staff find it hard to act on patient feedback?
Why do staff find it hard to act on patient feedback? https://www.careopinion.org.uk/resources/blog-resources/1-images/27e7956fe8e74cc6a38ffe3685560e65.png Care Opinion 0114 281 6256 https://www.careopinion.org.uk /content/uk/logos/co-header-logo-2020-default.pngQuestion from Care Opinion
Posted by James Munro, Director of Research & Development, Care Opinion, on
Response from Jane Danforth, Involvement & Experience Officer, Involvement, Experience and Volunteering Team, Nottinghamshire Healthcare NHS Trust on 5 Apr 2017 at 13:03
Hi James
In response to Sheard and colleagues, this resonates with us at Nottinghamshire Healthcare I’m pleased to say that our teams are given support and permission to make changes raised by patients, service users and carers locally. This gives staff ownership. They receive their team feedback via alerts and act on what is being said. Every story receives a personal reply. It has taken time and tenacity to embed this culture but it is so worth it.
Staff find it easier to relate to issues raised about their services without it always having to go ‘up the chain of command’ which often slows down the process of responding. Our staff can demonstrate that they feel confident by resolving things online openly.
Of course this is not as easy as it sounds. We receive stories that often challenge our services so we have to include senior staff when we really need to get to the heart of an issue. It is important to remember that we can't always change things for the better but the least we can do is listen and explain why this may not be possible.
Our Communications Team have always been supportive and this increases confidence for staff who may opt to use them as a sounding board along with Patient Opinion staff before responding as some stories can be complex involving multiple services.
The website functionality has developed enormously by working in Partnership with PO James, (soon to become CO!) Trigger alerts mean we can give staff a gentle 'nudge' when their planned changes are not followed through. This really helps us to bring the story to a conclusion. This function has improved on how we report on service changes to our Board of Directors.
Changes can often be very simple but make a huge difference. Listening and then acting is highlighted here in this story. I can't self -refer Can you Hear me?
Fast, simple and effective with a swift response by our Service Director Peter Caunt of Let’s Talk Wellbeing.
https://www.patientopinion.org.uk/opinions/353805
Thanks for listening to us at Notts.